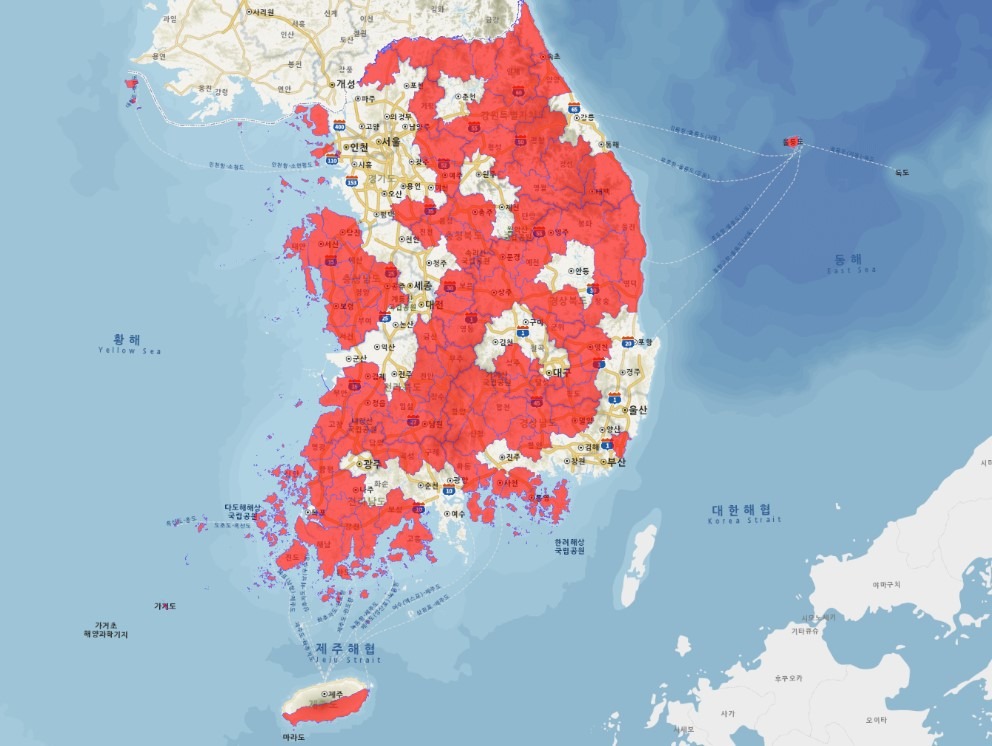
In South Korea today, regional disparities in essential and emergency medical services are deepening, and the resulting emergence of medically underserved areas has become a serious social issue. In particular, the collapse of medical infrastructure in rural areas has reached a level that threatens not just access to healthcare, but the very viability of those communities. The primary causes of this phenomenon are identified as the population imbalance brought about by rural depopulation and the concentration of population in the Seoul metropolitan area.

Rural depopulation leads to a continuous decline in the local population, resulting in decreased demand for medical services. This reduction in demand weakens the financial viability of medical institutions, ultimately causing an outflow of medical personnel and the downsizing or closure of facilities. According to South Korea’s emergency medical system status reports, many emergency medical institutions in rural areas are facing severe staffing shortages, making it difficult to provide adequate emergency care. In some regions, emergency services are reported to be completely unavailable at night or on holidays.
On the other hand, population concentration in the capital area exacerbates the uneven distribution of medical resources. Tertiary hospitals, medical schools, and research institutions are densely located in Seoul and Gyeonggi Province, accelerating the retention of medical talent and capital in the metropolitan region. As a result, rural areas fall significantly behind in both the quality and quantity of medical services compared to the capital area. This disparity can be life-threatening during emergencies, as securing the golden hour for patients in rural areas becomes difficult, leading to higher mortality rates.
The South Korean government is currently pursuing several policies to address the issue of medically underserved areas. For instance, the Ministry of Health and Welfare is applying region-specific reimbursement rates to support essential medical fields such as obstetrics and pediatrics and expanding financial support to strengthen the public healthcare role of regional medical centers. However, there is criticism that the current criteria for designating underserved areas focus excessively on physical distance and travel time, failing to adequately reflect actual medical demand and risk levels. Consequently, areas with low medical demand but high extinction risk receive disproportionate resources, while semi-urban towns near farming and fishing villages with relatively higher demand often fall outside the scope of such policies, creating blind spots.
To resolve these issues, a more integrated approach is needed—one that goes beyond simple budget allocation or medical staffing increases and links population redistribution policies with regional healthcare planning. Unless the rural population is maintained above a certain level, essential healthcare infrastructure cannot be sustained. In other words, healthcare can only exist where people live.
South Korea’s essential and emergency healthcare systems are currently facing a serious structural imbalance, and comprehensive, long-term policy efforts are required to address this challenge. Since healthcare is a public good directly related to the lives of citizens, what is needed is not a short-term fix but a systematic and long-term reform. The South Korean government must approach this issue not merely as a matter of “medical disputes” or “medical school quotas,” but through the lens of community sustainability and national balanced development.